Understanding Prostate Cancer: Signs and Treatment Options
The Importance of Early Detection
Prostate cancer is a significant health concern, particularly among men over the age of 50. Early detection plays a crucial role in effectively managing the disease and improving outcomes. Regular screenings, such as the prostate-specific antigen (PSA) test and digital rectal exams, are vital tools in identifying prostate cancer in its initial stages. These tests help detect abnormal growths or changes in the prostate gland, allowing for timely intervention.
Understanding the early signs of prostate cancer is essential. Symptoms may include difficulty urinating, frequent urges to urinate, especially at night, and blood in the urine or semen. However, it’s important to note that these symptoms can also be caused by non-cancerous conditions, such as benign prostatic hyperplasia (BPH). Therefore, consulting a healthcare professional for accurate diagnosis and advice is crucial.
Early detection not only improves the chances of successful treatment but also offers a wider range of treatment options. When prostate cancer is caught early, less invasive treatments may be possible, reducing the impact on a patient’s quality of life. Therefore, raising awareness about the importance of regular screenings and recognizing symptoms is key to combating prostate cancer effectively.
Risk Factors and Prevention
Several risk factors increase the likelihood of developing prostate cancer. Age is a primary factor, with the risk rising significantly after age 50. Family history also plays a role; men with close relatives who have had prostate cancer are at a higher risk. Additionally, certain genetic mutations have been linked to an increased risk.
While some risk factors like age and genetics cannot be changed, lifestyle choices can influence the risk of developing prostate cancer. Maintaining a healthy diet rich in fruits, vegetables, and whole grains, while limiting red meat and high-fat dairy products, may help lower the risk. Regular physical activity and maintaining a healthy weight are also beneficial in reducing the likelihood of developing prostate cancer.
Preventive measures are not guaranteed to eliminate the risk, but they can contribute to overall health and well-being. It’s important for individuals, especially those with risk factors, to engage in regular health check-ups and discussions with their healthcare providers about prostate cancer screening options.
Diagnosis and Staging
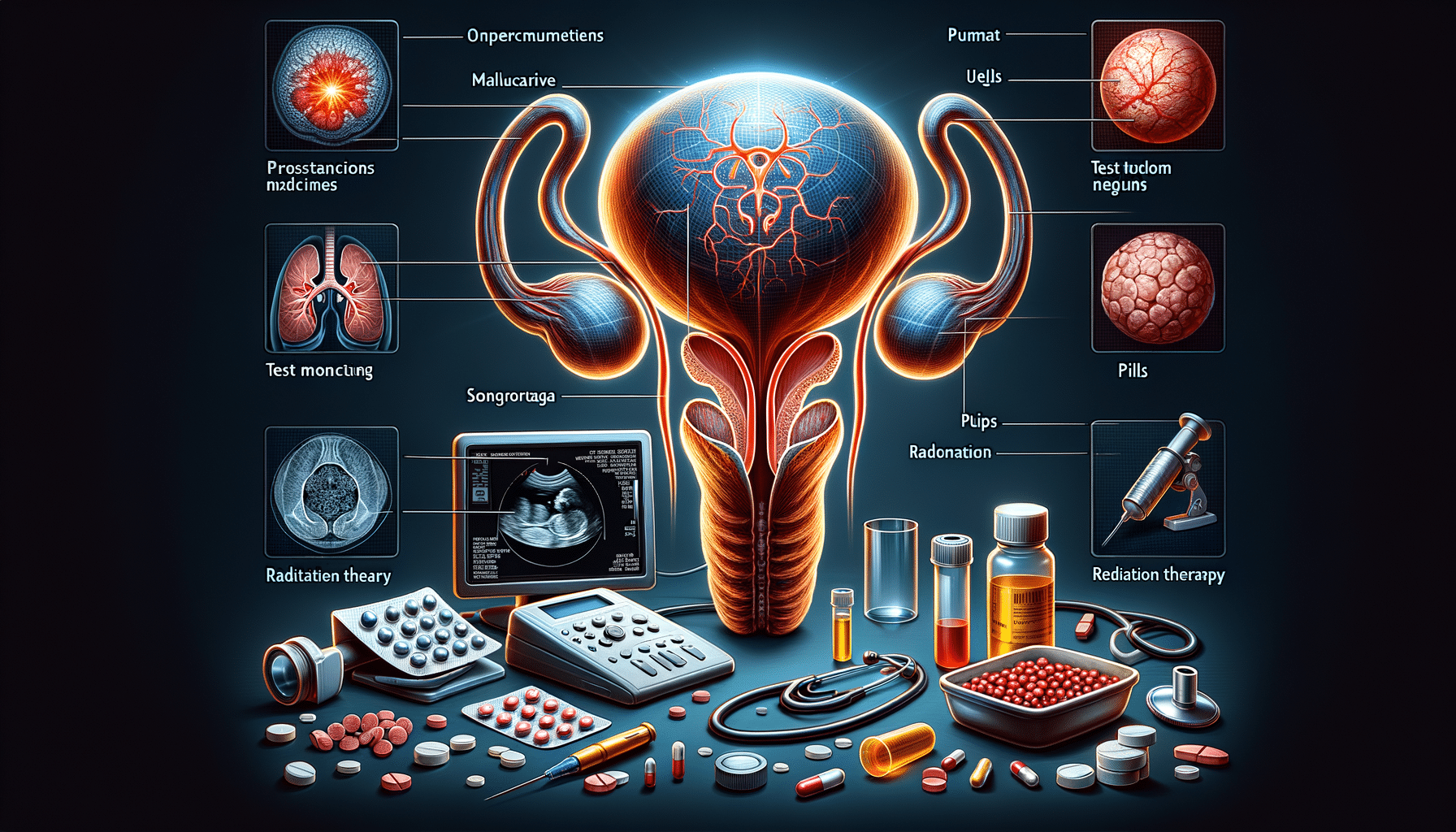
When prostate cancer is suspected, a series of tests are conducted to confirm the diagnosis and determine the stage of the cancer. The initial step often involves a PSA test and a digital rectal exam. If results indicate potential cancer, a biopsy may be recommended to examine prostate tissue under a microscope.
Once diagnosed, staging the cancer is crucial to guide treatment decisions. Staging involves assessing the size of the tumor, whether it has spread to nearby lymph nodes or other parts of the body, and the Gleason score, which indicates the aggressiveness of the cancer cells. Imaging tests like MRI, CT scans, or bone scans may be used to help determine the extent of the cancer.
Understanding the stage of prostate cancer helps in tailoring treatment plans to the specific needs of the patient. It also provides valuable information about the prognosis and potential outcomes, enabling patients and healthcare providers to make informed decisions about the best course of action.
Treatment Options
Treatment for prostate cancer varies depending on the stage and grade of the cancer, as well as the patient’s overall health and preferences. Common treatment options include active surveillance, surgery, radiation therapy, hormone therapy, and chemotherapy.
Active surveillance is often recommended for low-risk, slow-growing cancers. This approach involves regular monitoring of the cancer without immediate treatment, allowing patients to avoid or delay the side effects of more aggressive treatments. Surgery, such as a prostatectomy, may be considered for localized cancers and involves the removal of the prostate gland.
Radiation therapy uses high-energy rays to target and kill cancer cells. It can be an option for localized or advanced prostate cancer. Hormone therapy aims to reduce or block the production of testosterone, which fuels the growth of prostate cancer cells. Chemotherapy, typically used for advanced cancer, involves the use of drugs to destroy cancer cells throughout the body.
Each treatment option has its benefits and potential side effects, and the choice depends on various factors, including the cancer’s stage and the patient’s preferences. Collaborating with a healthcare team to discuss the pros and cons of each option is essential for making an informed decision.
Living with Prostate Cancer
Living with prostate cancer involves managing both the physical and emotional aspects of the disease. Support from healthcare professionals, family, and support groups can be invaluable in navigating the challenges associated with prostate cancer.
Patients may experience physical side effects from treatments, such as fatigue, urinary incontinence, and sexual dysfunction. Addressing these issues with healthcare providers can help find effective management strategies and improve quality of life.
Emotionally, a cancer diagnosis can be overwhelming. It’s important for patients to express their feelings and seek support from loved ones or mental health professionals. Joining support groups can also provide a sense of community and understanding from others who are going through similar experiences.
Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can support overall well-being and recovery. Staying informed about the latest advancements in prostate cancer research and treatments can empower patients to make proactive decisions about their health.