Explore Atrial Fibrillation Treatment Guidelines
Understanding Atrial Fibrillation
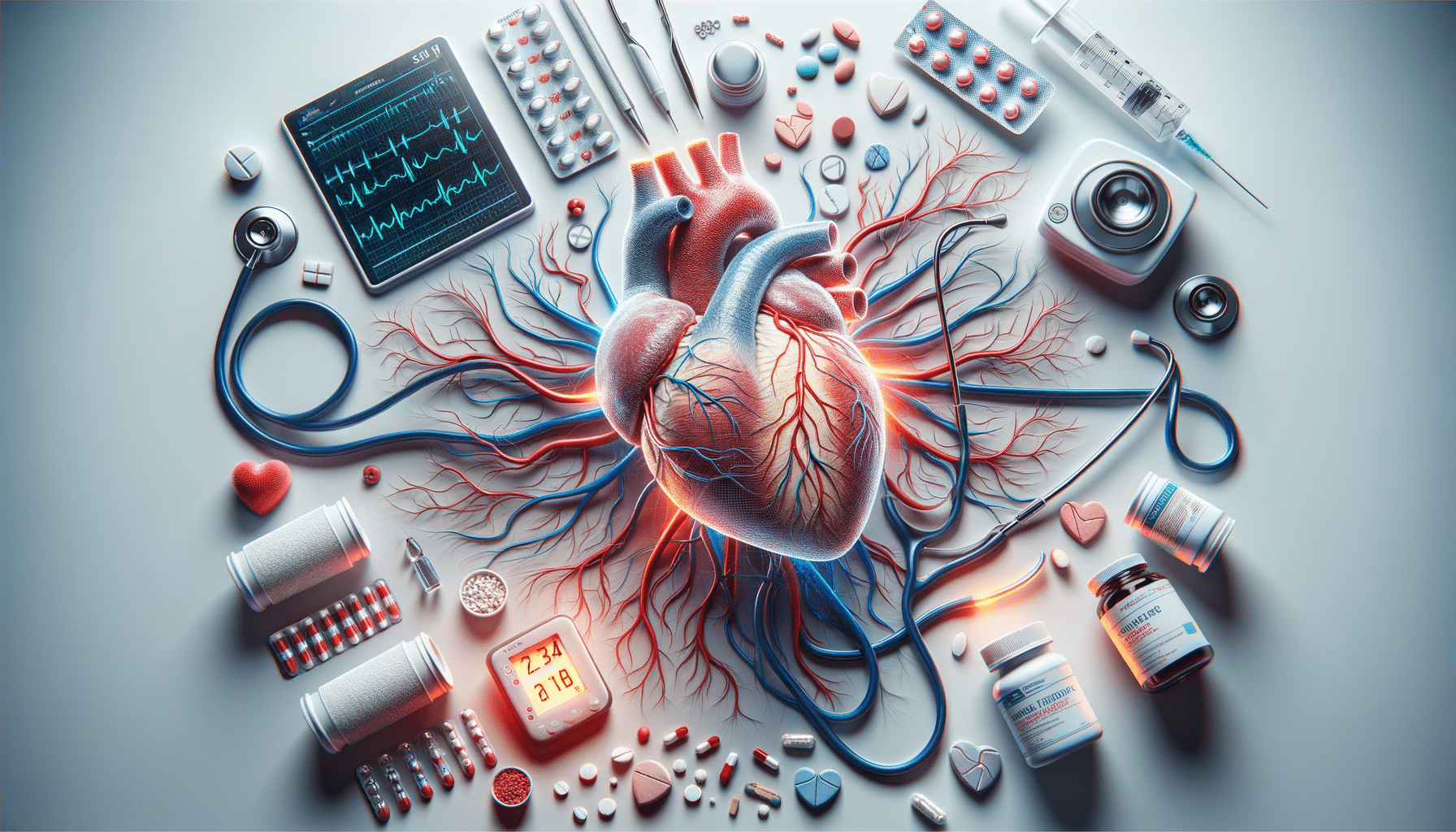
Atrial fibrillation, often abbreviated as AFib, is a common heart condition characterized by an irregular and often rapid heart rate that can increase the risk of strokes, heart failure, and other heart-related complications. In a healthy heart, electrical signals are synchronized to ensure a steady heartbeat. However, in atrial fibrillation, these signals become chaotic, causing the heart’s upper chambers, the atria, to quiver or fibrillate. This condition affects millions of people worldwide and becomes more prevalent with age. Understanding the nature of atrial fibrillation is crucial for effective management and treatment.
Several factors contribute to the onset of atrial fibrillation, including high blood pressure, heart disease, and lifestyle factors such as excessive alcohol consumption and smoking. Symptoms can vary widely among individuals, with some experiencing noticeable heart palpitations, fatigue, or shortness of breath, while others may remain asymptomatic. The variability in symptoms underscores the importance of regular health check-ups, especially for those with risk factors.
Diagnosing atrial fibrillation typically involves an electrocardiogram (ECG) to detect irregular heart rhythms. In some cases, additional monitoring may be required to capture intermittent episodes of AFib. Early diagnosis and intervention are vital to prevent complications and improve quality of life for those affected.
Symptoms and Diagnosis of Atrial Fibrillation
Recognizing the symptoms of atrial fibrillation is essential for timely diagnosis and treatment. Common symptoms include a fluttering or thumping sensation in the chest, known as palpitations, along with fatigue, dizziness, and shortness of breath. In more severe cases, individuals may experience chest pain or fainting spells. However, it’s important to note that some people with atrial fibrillation may not exhibit any symptoms, making regular medical check-ups crucial for early detection.
The diagnostic process for atrial fibrillation usually begins with a physical examination and a review of the patient’s medical history. An electrocardiogram (ECG) is the primary tool used to detect the irregular heartbeats characteristic of AFib. In cases where atrial fibrillation is suspected but not immediately apparent, doctors may recommend a Holter monitor or an event recorder to capture intermittent episodes over a more extended period.
In addition to these diagnostic tools, healthcare providers may conduct blood tests to assess thyroid function and other potential contributing factors. Imaging tests like an echocardiogram may also be used to evaluate the heart’s structure and function. The combination of these diagnostic approaches helps in formulating an effective treatment plan tailored to the individual’s needs.
Medications for Managing Atrial Fibrillation
Medications play a pivotal role in managing atrial fibrillation, aiming to control heart rate, restore normal rhythm, and prevent complications such as stroke. The choice of medication depends on various factors, including the severity of symptoms, underlying health conditions, and the individual’s overall health profile.
One of the primary goals in treating atrial fibrillation is to control the heart rate. Beta-blockers and calcium channel blockers are commonly prescribed to help achieve this. These medications work by slowing down the heart rate, allowing the heart to function more efficiently. In some cases, antiarrhythmic drugs may be used to restore and maintain a normal heart rhythm.
Preventing stroke is another critical aspect of managing atrial fibrillation. Blood thinners, or anticoagulants, are often prescribed to reduce the risk of blood clots forming in the heart’s atria, which can travel to the brain and cause a stroke. It’s essential for patients to work closely with their healthcare providers to determine the most suitable medication regimen, as these drugs can have significant side effects and require careful monitoring.
Common Treatment Options for Atrial Fibrillation
Beyond medications, several treatment options are available for managing atrial fibrillation. These options are tailored to the individual’s specific condition and may include lifestyle modifications, medical procedures, or a combination of both. The primary aim is to improve heart function, reduce symptoms, and prevent complications.
Lifestyle changes can significantly impact the management of atrial fibrillation. Patients are often advised to adopt heart-healthy habits such as regular exercise, a balanced diet, and avoiding excessive alcohol and caffeine intake. Stress management techniques, including yoga and meditation, may also be beneficial in reducing episodes of AFib.
For individuals who do not respond adequately to medications or lifestyle changes, medical procedures may be considered. Cardioversion, a procedure that uses electrical shocks to restore a normal heart rhythm, is one option. Another procedure, catheter ablation, involves destroying the heart tissue responsible for the irregular signals. In some cases, a pacemaker may be implanted to regulate the heart’s rhythm. Each of these treatment options has its own set of benefits and risks, and decisions are made based on a comprehensive evaluation of the patient’s condition.
Living with Atrial Fibrillation
Living with atrial fibrillation requires ongoing management and lifestyle adjustments to minimize symptoms and reduce the risk of complications. Education and awareness are vital components in empowering patients to take an active role in their health care. Understanding the condition, its triggers, and treatment options can lead to better health outcomes and an improved quality of life.
Patients with atrial fibrillation should maintain regular follow-ups with their healthcare providers to monitor their condition and adjust treatment plans as needed. This ongoing care is crucial for detecting any changes in the heart’s rhythm or function and ensuring that medications are effective and well-tolerated.
Support from family, friends, and support groups can also play a significant role in managing the emotional and psychological aspects of living with a chronic condition. Sharing experiences and coping strategies with others who have atrial fibrillation can provide valuable insights and encouragement. Ultimately, with proper management and support, individuals with atrial fibrillation can lead fulfilling and active lives.